Diversity issues in medicine: beyond black and white
Written by: Cassandra Hui
The issue of having enough diverse representation in clinical trials and health research is not a new conversation. We can trace diversity issues back to the early days of immigration for low-wage workers as leading causes for the systemic issues with health care today. Basically, when immigrant workers came to the North Americas to take on low paying jobs access to healthcare, politics and other freedoms were inaccessible as seen as a right only for those who had born citizenship in a country. In a sense,“access to health and other services remains intrinsically linked to claims of citizenship, with health and social care professionals increasingly required by the state to act as a second (often reluctant) line of immigration control.”(Ahmad, Bradby, 2008)
Although inequality in health has been studied, highlighted and reported over the years, the problem has been amplified with a global need for vaccination trials seen over the last year. Why is it more important than ever? Rolling out a global vaccine to billions of people from different ethnicities and backgrounds needs to be representative and accurate in order to understand if potential medicines work and what their side effects are across all races, genders and identities.
“Diverse racial/ethnic representation in COVID-19 vaccine trials is important because drugs and vaccines can differentially affect groups reflecting variation in underlying experiences and environmental exposure.” (kff.org)
Being “color-blind”
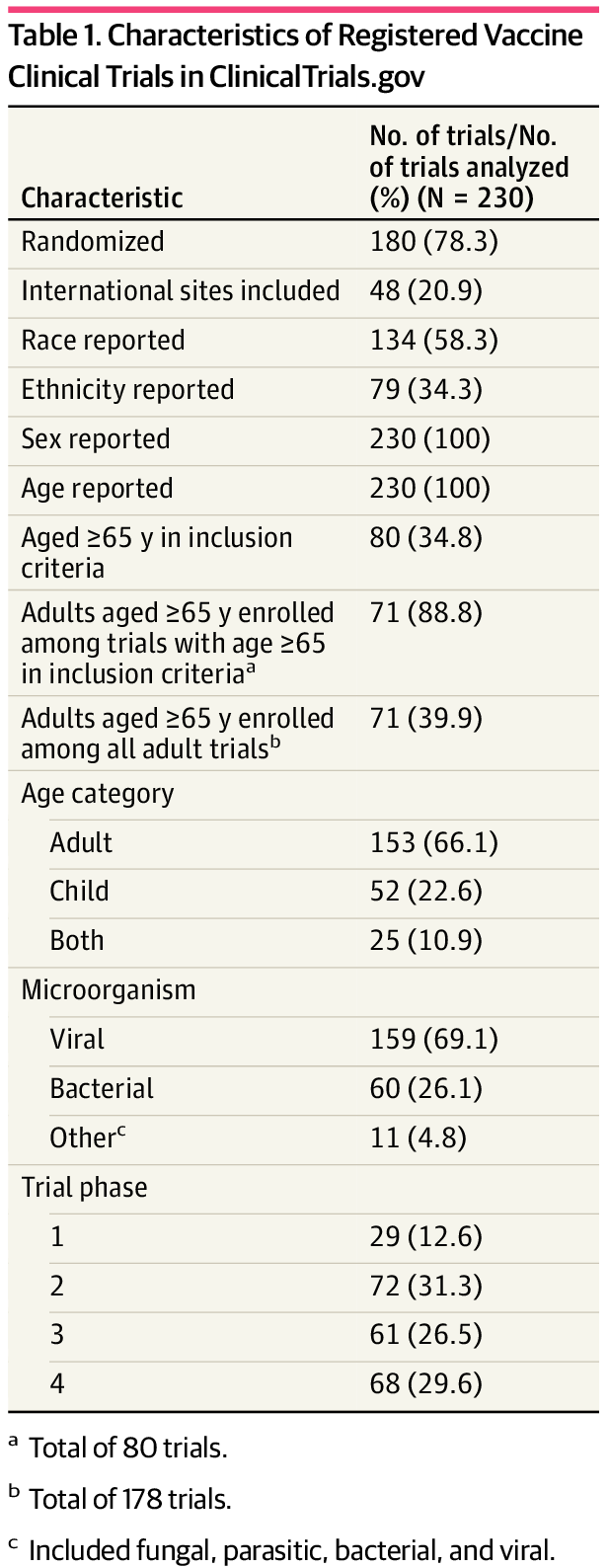
A recent study reported that 60% of trials do not report racial/ethnic data and yet we know that on average, less than 10% of participants in cancer trials, for example, will represent people who are of BIPOC backgrounds. A JAMA study took the available vaccine clinical trials during the pandemic to measure what representation each group had. The study’s findings were “that among US-based vaccine clinical trials, members of racial/ethnic minority groups and older adults were underrepresented, whereas female adults were overrepresented. These findings suggest that diversity enrollment targets should be included for all vaccine trials targeting epidemiologically important infections.” (JAMA network)
Source: Jama Network Open
How do we start to increase diversity in clinical trials?
The key to starting to move the needle on representation in health and clinical trials is around access.
Access to clinical trials physically
When studies are conducted, the physical location matters. In a study by Cheng and Levy, “elderly patients, who often have difficulty traveling for care, had to travel more frequently than the average patient. In addition to the sheer number of times patients must travel to medical centers for care, patients also perceive commuting as a burden. In a survey of 1053 patients regarding factors that contributed to their treatment burden, 41% expressed that they had difficulty adapting to new routines for care that involved planning and organizing travel. Additionally, 30% of patients surveyed indicated they had difficulty with access to health care centers citing distance and parking as barriers to receiving care.”
In our patient interviews with caregivers, we also received feedback that for those who were unable to drive because of severe illness or other factors, they depended that their caregiver be able to help them commute, and in households where the working caregiver’s income was a necessity, applying to participate in clinical trials wasn’t an option.
With the pandemic, we saw a rise in the use of mobile health units and were working closely with other organizations finding new ways to conduct clinical trials. The asset of mobile health and the move toward decentralized trials, is an exciting development.
2. Access to culturally sensitive concerns about clinical trials
Working to become aware of some of the real hesitations for patient fears about clinical trials is a good way to start addressing those concerns that are individual and unique to individuals. People whose trust has been broken in previous generations often pass those ideas about doctors and healthcare forward in how they personally handle disease in the family like the infamous Tuskegee Trials. Sensitivities around the view of death and perception of palliative and hospice care in Chinese cultures who see palliative care centres as “repositories of ‘inauspicious care’ in which opportunities for achieving an appropriate or good death was limited,” and therefore prefer to spend their final days in a hospital that is viewed in a much higher regard. (Seymour, Payne, Chapman and Holloway, 2008)
3. Access to understanding
Access to information about one’s personal health is increasing and the demand from patient’s to access their personal health information conveniently has shifted. However, a patient is typically thrust into a position of understanding their health and the complexities of their diagnosis with limited or no scientific or medical knowledge. Practitioners have made significant efforts to explain processes or diagnoses in plain language but whatever happens in the late hours between Dr. Google and a patient is where discrepancies and misinformation is likely to occur. Clinical trials have remained geared towards the doctors who treat vs. the patient needing to be treated. Using technology, making it easy for patients to understand clinical trials and to understand what they are enrolling in alleviates part of the fears and burden. Patients want information but they need to be able to understand it. *(Heal Mary’s initial step was to translate medical jargon to plain language)
Final thoughts
These problems are not easily solved due to the many players involved in the healthcare system along with deep rooted systemic issues but we know that the ability to change and take small steps to increasing access for patients will be significant.
The disruption in the past year to health has been a pivotal one with the ability to build on this for future teamwork in clinical trials and engaging a patient as the most important piece of the process. Though the last year has highlighted significant issues with the current clinical trial model, we all remain hopeful about the significant changes that will occur After all, “All great changes are preceded by chaos.” — Deepak Chopra
To find out more about Heal Mary and our mission to empower patients, visit our website here.